Most people don’t consider sleep when they think about their allergies.
They think about pollen, pets, or peanut butter, but rarely about their pillow. And that’s a mistake.
Poor sleep doesn’t just make you groggy or irritable. It rewires your immune system for the worse. And if you already have allergies, it can turn a mild nuisance into a daily battle.
Nobody talks about this because there’s no profit in prescribing sleep, even though studies show that 40–50% of allergy and asthma patients struggle with some kind of sleep disorder.
So let’s look at what the science actually says about this overlooked connection, and why your best allergy treatment might start with a better night’s rest.
Why Sleep Is the Missing Piece in Allergy Care
When I meet new patients, I always ask about sleep.
A person’s sleep, or lack thereof, reveals more than almost any lab test. If you’re not sleeping well, your oxygen levels dip. Your heart, kidneys, and brain go hungry for air. Imagine trying to run a car with half the fuel line pinched; that’s your body on sleep deprivation.
And if you add nasal congestion or sinus pressure from allergies, well, now you’re trying to breathe through a blocked straw all night long.
This means you’ll wake up tired, inflamed, and already behind on healing before the day begins.
The Allergy–Sleep Cycle: A Vicious Loop
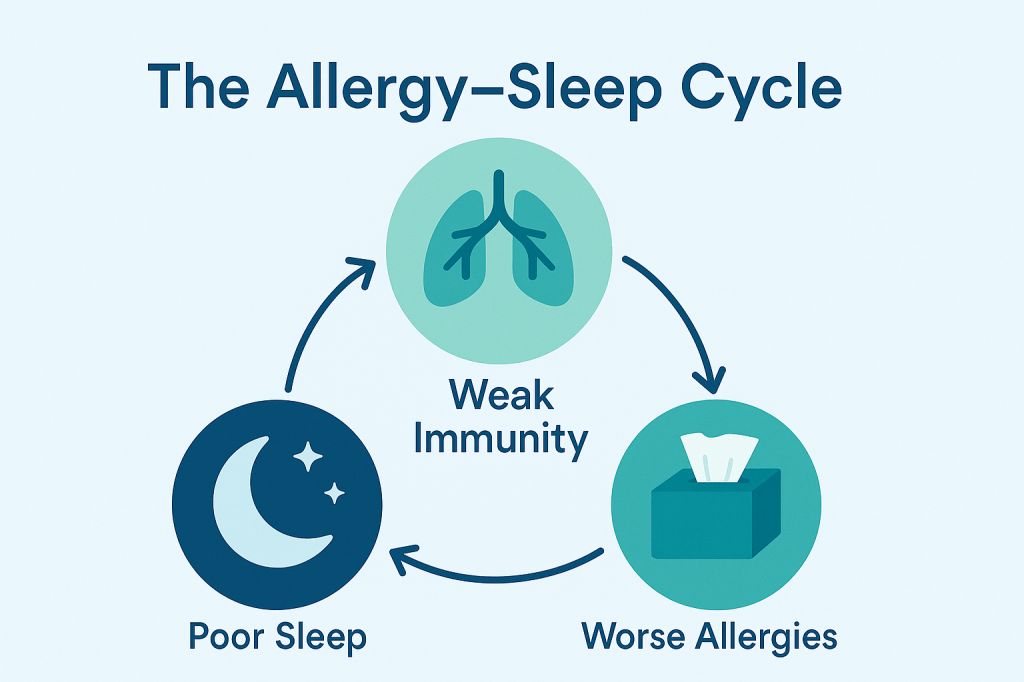
And here’s the frustrating part: allergies make sleep worse, and poor sleep makes allergies worse.
They feed off of each other.
When your nose is stuffed, you mouth-breathe, which dries your throat and triggers coughing. That coughing wakes you up. Now, you lose deep sleep, which weakens your immune regulation.
And that weakened immune system turns around and amplifies your allergic reactions.
The research we have on this backs this up.
Sleep deprivation shifts your immune balance toward what’s called the TH2 response, which is the arm of your immune system responsible for allergies and inflammation. That means more histamine, more cytokines, and more miserable mornings.
Cytokines: The Middlemen of Misery
Cytokines are your body’s messengers, essentially little text alerts fired between immune cells to coordinate what kind of defense your body mounts.
When you lose sleep, your body starts sending the wrong messages. Levels of interleukin-4 and interleukin-13 (two key TH2 cytokines) surge. That shift pushes your immune system toward the TH2 side, the arm responsible for asthma, wheezing, nasal congestion, and hay fever.
In other words, the more TH2 activity you have, the more your airways tighten, the more you cough, and the more your allergies flare.
This also raises your IgE levels, the antibody that drives allergic reactions. Over time, chronic sleep loss may even make airway inflammation less responsive to corticosteroids, which is one reason exhausted patients often feel their asthma meds “don’t work like they used to.”
These same cytokines are the exact targets of pricey biologic drugs like Dupixent, which try to block that TH2 response. But here’s the good news: before spending thousands to quiet those molecules, you should focus on getting better sleep.
Sleep is the cheapest and most effective immunotherapy you can get.
The Overlooked Role of Sleep Apnea
Sleep apnea is another silent allergy amplifier.
Even mild apnea can drop your nighttime oxygen levels into the 70s or 80s. Healthy numbers should hover near 95–98%. So when oxygen dips that low, your body pays the price: your organs—heart, kidneys, brain—all work in survival mode, which causes your inflammation to skyrocket.
And you don’t have to snore loudly or wake up gasping to have sleep apnea. Sometimes the only clues are dry mouth in the morning, fatigue that coffee can’t fix, or a bed partner who notices pauses in your breathing.
I recommend a simple home sleep study, even with a small sensor on your thumb, to identify the problem. It’s cheap, and with treatment, whether through a CPAP, dental appliance, or implantable device, it can be life-changing.
Lifestyle Habits That Quietly Ruin Your Sleep
Most patients don’t realize how many daily habits sabotage their sleep.
Screen time is a big one. Blue light from phones and TVs tells your brain it’s noon even when it’s midnight.
Then there’s caffeine, especially the “just one cup” after dinner.
Perhaps most surprising to my patients is having alcohol to help go to bed. While it helps you fall asleep, it will wreck your sleep quality three hours later. That 2 a.m. wake-up call? That’s your dopamine levels crashing as the effects of wine disappear.
Even a big meal before bed can backfire. Reflux sneaks in, especially if you’re lying flat. That’s why I often recommend a wedge pillow or an adjustable bed. Elevating your head just a few inches can reduce both congestion and reflux.
Obesity, Sleep, and Allergy: The Triple Threat
Obesity, sleep deprivation, and allergies feed off each other like wolves in a pack.
Extra weight narrows the airway, increases inflammation, and raises your risk of sleep apnea. Less sleep increases cravings and disrupts metabolism, making weight loss harder.
And both make asthma and allergic rhinitis worse.
While that may sound hopeless, there’s a simple fix: Lose 10–15 pounds and improve your sleep hygiene, and your allergy symptoms can noticeably calm down.
The Peanut Problem: Sleep Deprivation and Food Allergies
This one shocked even me.
Recent studies show that sleep deprivation increases the severity of allergic reactions to peanuts by 48%. Almost fifty percent. That’s the difference between a mild hive and a full-blown anaphylactic emergency.
When you don’t sleep, your body loses its ability to regulate hypersensitivity. The same exposure that caused a sniffle last week might trigger a severe reaction today.
Unfortunately, this hypersensitivity extends across the board: eczema, asthma, hay fever, and rhinitis.
If you sleep less, you’ll react more.
Practical Steps to Sleep (and Breathe) Better
If you’re an allergy patient who’s dragging through the day because you barely slept, start here:
1. Elevate your head.
Sleep on an incline. Use a wedge pillow or raise the head of your bed a few inches. This helps air move freely through your nose and throat and also reduces reflux, which is a hidden allergy aggravator that creeps up when you lie flat.
2. Skip big meals before bed.
Finish dinner at least two hours before sleep. Heavy or late-night meals increase reflux, which inflames the throat and worsens congestion.
3. Ditch the “nightcap” myth.
That glass of wine might knock you out fast, but it sabotages your deep sleep later. Alcohol briefly boosts dopamine, then crashes it around 2 a.m., jolting you awake and leaving you groggy.
4. Rethink sedation.
Over-the-counter “PM” antihistamines make you drowsy, not rested. Sedation isn’t real sleep. Those drugs may worsen airway dryness and leave you more congested by morning.
5. Try mechanical help.
A simple oral appliance that gently moves your lower jaw forward can keep your airway open, especially if your tongue tends to fall back during sleep. If that’s not enough, modern CPAPs are smarter and quieter than ever, automatically adjusting airflow when you stop breathing. For those who can’t tolerate CPAP, newer implantable options like the Inspire device stimulate the tongue muscles just enough to prevent obstruction.
6. Check your oxygen.
Before jumping to devices, start small. A home sleep study or even a simple fingertip oxygen monitor can reveal if your nighttime oxygen dips below 90%.
No matter what you do, don’t lose hope.
Almost every patient I’ve treated eventually finds something that helps, such as losing a little weight, eating earlier, doing a home sleep study, or getting the right airway support.
When your sleep steadies, your energy rises, your mood evens out, and your allergies start to quiet. Just as a rising tide lifts all ships, lowering the tide of sleeplessness calms every storm in the body: asthma, congestion, fatigue, and inflammation.
Real healing begins in those quiet hours, where your head is on the pillow, body at rest, and your lungs are finally, fully breathing again.